ARTÍCULO ORIGINAL
doi: http://dx.doi.org/10.7705/biomedica.v35i3.2634
1 Grupo de Alergología Clínica y Experimental, IPS Universitaria, Universidad de Antioquia, Medellín, Colombia
2 Fundación para el Desarrollo de las Ciencias Médicas y Biológicas, Cartagena, Colombia
3 Instituto de Investigaciones Inmunológicas, Universidad de Cartagena, Cartagena, Colombia
Author’s contributions:
Jorge Sánchez generated the main idea of the study.
All authors contributed equally to the preparation and drafting of the manuscript.
Recibido: 12/12/14; aceptado: 07/04/15
Introduction: Among allergic patients, pet avoidance is commonly recommended. It is difficult for patients to accomplish this because of their emotional attachment to the pets, and its effectiveness is controversial.
Objective: To explore the applicability and effectiveness of pet avoidance measures among sensitized patients.
Materials and methods: We evaluated 288 patients with asthma, rhinitis, conjunctivitis and/or dermatitis using skin prick test to measure their sensitization to cats, dogs and other animals to which they were exposed. Exposure to animals was evaluated in each patient (pets at home, frequent indirect exposure or no exposure). In those patients sensitized to animals some avoidance measures, such as removing pets from home and preventing indirect exposure, were recommended. On the following two appointments, we evaluated patients´ fulfillment of these recommendations.
Results: Sensitization to cats, dogs and birds was high (9%, 48%, 14%, respectively), as well as direct and indirect exposure (30%, 46%, 24%, respectively). Most patients denied contact with other animals (horses, hamsters, rabbits or cows), and sensitization to them was low. During the follow-up of patients sensitized to their pets at home (n=50), most of them refused to remove them from their house due to emotional attachment, and only two followed this recommendation.
Conclusions: High exposure to animals could explain the frequency of sensitization to pets in this population. However, emotional attachment and prevalent indirect exposure to animals among sensitized patients make avoidance recommendations impractical or impossible to achieve.
Key words: Allergy, pets, dog, cat, horse, birds, sensitization.
doi: http://dx.doi.org/10.7705/biomedica.v35i3.2634
Evitación de mascotas en casos de alergia. ¿Es factible lograrla?
Introducción. Entre los pacientes alérgicos se recomienda comúnmente la evitación de mascotas; sin embargo, es difícil que los pacientes cumplan con esta recomendación debido al apego emocional y, además, su efecto clínico no es claro.
Objetivo. Explorar la aplicabilidad de las medidas de evitación entre pacientes sensibilizados a mascotas .
Materiales y métodos. En 284 pacientes con asma, rinitis, conjuntivitis y dermatitis, se evaluó la sensibilización a gatos, perros y otros animales mediante pruebas de punción epidérmica. Se evaluó, igualmente, el nivel de exposición a animales (mascotas en la casa y exposición indirecta frecuente). A aquellos pacientes sensibilizados a los animales, se les recomendaron medidas de evitación como retirar la mascota de la casa y evitar la exposición indirecta. En las dos citas médicas siguientes se evaluó el cumplimiento de estas recomendaciones.
Resultados. La sensibilización a gatos, perros y aves fue alta (9, 48, y 14 %, respectivamente), al igual que la exposición directa o indirecta a estos animales (30, 46, 24 %, respectivamente). La mayoría de los pacientes negó el contacto frecuente con otros animales (caballos, hámsteres, conejos, vacas) y la sensibilización a estos fue baja. La mayoría de los pacientes sensibilizados a su propia mascota (n= 50) se rehusó a retirar la mascota de la casa y solo dos de ellos siguieron la recomendación de hacerlo.
Conclusiones. La exposición frecuente a los animales podría explicar la gran frecuencia de sensibilización a las mascotas en esta población. Sin embargo, el apego emocional y la exposición indirecta frecuente, hacen que las recomendaciones de evitación sean imprácticas o casi imposibles de lograr.
Palabras clave: hipersensibilidad, inmunización, mascotas, perros, gatos, caballos, aves.
doi: http://dx.doi.org/10.7705/biomedica.v35i3.2634
The frequency of atopy and allergic diseases like asthma, rhinitis and conjunctivitis is high and it seems that the incidence is growing, especially in developing countries. (1) On the other hand, the number of families with pets at home is also increasing. The risk of prolonged exposure to pets or its effectiveness as a protective factor for allergic diseases is still under intense debate; however, for patients with suspected allergic diseases, clinical guidelines recommend to avoid such exposure. (2) This recommendation seems obvious, but most patients face difficulties in achieving this goal and the clinical effectiveness of such recommendations is not clear. (3)
Cats and dogs are one of the main causes of sensitization in Europe, (4) which has also been observed in Medellín, Colombia. (5) In this study we explored the applicability and effectiveness of avoidance measures among patients sensitized to pets.
Materials and methods
Study design and population selection
We carried out a prospective ambispective study. Some patients were selected from a population of individuals diagnosed with asthma, rhinitis or atopic dermatitis who attended the Universidad de Antioquia´s allergy service (Medellín, Colombia) from June, 2012 , to March, 2014 , and required a skin prick test to clarify possible environmental triggers.
Disease diagnosis was established according to the Global figuInitiative for Asthma guidelines (www.ginasthma.org), the Allergic Rhinitis and its Impact on Asthma guidelines, (6) the Ocular Allergy Latin American Consensus for Conjunctivitis (7) and the Hanifin and Rajka criteria for atopic dermatitis. (8) Patients were considered as having a multisys temic phenotype if they showed both respiratory and cutaneous symptoms. To consider patients as allergic, they had to be sensitized to one or more allergens of clinical relevance based on their clinical history or a provocation test.
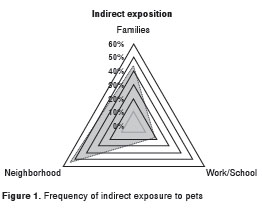
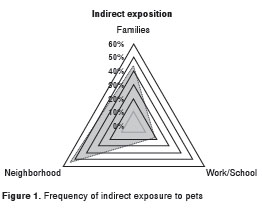
During the appointment for the skin prick test, patients were asked about suspected triggers and the presence of pets at home or indirect exposure to common animals. After the prick test, patients received verbal and written information about environmental control for possible trigger sources. Patients were categorized in subgroups according to the variables related to exposure to pets and atopy. The study arbitrarily defined that frequent indirect exposure occurred when a patient had no pets at home but had contact with animals for at least 2 hours a week or 30 minutes a day or 3 days a week (figure 1). All patients had at least two subsequent follow-ups 3 to 5 and 6 to 9 months after the prick test. In the two follow-up appointments, patients were asked if they had followed the recommendations, especially avoidance of pets at home.
Skin prick test
Using skin prick tests, patients were exposed to standardized commercial extracts (Inmunotek Laboratory, Madrid, Spain). The panel of allergenic extracts used included the mites Blomia tropicalis (Blo t), Dermatophagoides pteronyssinus (Der p), and Dermatophagoides farinae (Der p), pet dander (cat and dog), the fungi Asperllilus fumigatus, Cladosporium herbarum and Alternaria alternata , feather from canaries, doves and parakeets, insects (cockroach, mosquito and ant), and pollen grains (herbs, cereals, flowers, grasses and trees). We followed the international recommendations for prick test reading: we considered a wheal as positive if it was 3 mm bigger than the negative control. (4, 9) Before the test, all patients discontinued the use of antihistamines or other drugs as indicated.
All patients tested for Blo t, Der p, Der f, and cat and dog dander were included in the study . The study probed additional extracts in patients who had contact with other animals (e.g., birds, horses and hamsters). Other animals such as hens, doves, parakeets and canaries were probed according to the patients´ level of exposure to them.
Statistical analyses
Analyses were performed with IBM SPSS ® , version 21 for Windows. The results and the general characteristics of patients were expressed as frequency percentages in absolute numbers. We used correlation and chi-square tests or multivariate logistic regression to assess the difference between groups.
Ethical considerations
Institutional approvals by the IPS Universitaria and Universidad de Antioquia´s ethics committees were obtained. No experiments were performed on humans or animals during this research. Authors declare that no patients´ data appear in the article.
Results
Population characteristics
The study included 284 patients of whom 149 were women (table 1). Age mode, mean, and median were 11, 20 and 14 years, respectively. Most patients had respiratory diseases (90%), and 38 (13%) of them both respiratory and cutaneous conditions; 227 patients (80%) had atopy and the main sensitization source were dust mites (218 patients, 76%); 173 patients ( 61% ) were sensitized to at least two different groups of sources (polysensitized).
Sensitization to animals
One hundred and fifty five patients (53%) were positive at least to one animal. The most frequent allergenic sources among pets were dogs with 136 sensitized patients (48%), followed by cats with 27 sensitized patients (9,5%). According to the patients´ clinical records, 78% of those sensitized to an animal were sensitized to the one they suspected was the trigger. On the other hand, 18 patients who were positive to cats were positive to dogs too. Six patients were positive to horses and one to rabbits, and all seven of them were positive to cats and dogs, too; 33 patients (14%) were positive to birds, of whom 24 were also positive to cats or dogs; 135 of the patients positive to dogs (99%) were sensitized to mites, and all the patients positive to cats were also positive to mites (table 2).
Exposure to pets
Taking into consideration that all the study population had respiratory or cutaneous symptoms, it was not possible to evaluate if there was a relationship between exposure to pets and symptoms, but we explored the relationship between exposure and sensitization. One hundred and forty patients (49%) had at least one pet at home (table 3). The most common ones were dogs (n=80), cats (n=50) and birds (n=28). Other animals like horses, pigs and hamsters were less frequent (n=38 ). The patient who was positive to rabbits had one at home and four out of the six patients positive to horses had a frequent contact with this animal; however, there were few patients who had contact with these animals, so it was not possible to evaluate if the association with sensitization was statistically significant. No significant relationship between having cat or dog at home and sensitization was observed, but we did register a direct association between having birds at home and sensitization to them (p=0.01) (table 4).
Pet avoidance
A total of 50 patients were sensitized to the pet they had at home: 38 to dogs, four to cats and eight to birds. These patients were instructed to avoid their pets at home for the prick test. Sixty-six percent of patients sensitized to their pets refused to remove their pet from home even after a positive result in the prick test and the clinical recommendations. In the first follow-up after the prick test, 46 patients (92%) still had their pets and in the second appointment, 44 (88%), which means that only six patients (12%) were not exposed to their pets: three patients because they lost their pet, one pet died and only two patients followed the medical recommendation.
Among patients with high indirect exposure, most (152 patients) said that they had tried to reduce contact with their pets (94%), but 84% said that they could not avoid the source or sources of indirect exposure (44%: at home, 18%: at work/school, 54% in the neighborhood). Four patients got a new pet during the follow-up, two of them a pet they were sensitized to (figure 1).
Discussion
Taking into consideration that the difference in sensitization patterns may vary according to geographical and socio-cultural conditions, (10- 12) it is appropriate to put into perspective some geographical aspects of the study area before discussing the results of the study. The Aburrá Valley area is a basin located between two moun tain ranges at an altitude of 1,479 meters above sea level. Given its location between mountains, there are usually mild winds that favor the transport and concentration of particulates such as those arising from epithelium, droppings and feathers, thus increasing the exposure to animals among people without pets. According to the Colombian Ministerio de Salud y Protección Social (www.minproteccionsocial.gov.co), and the Regional Animal Protection Society ( www.spac-05.tripod.com), in Medellín there is a pet in one of every three houses (dogs, 86% and cats, 17%), which suggests that there is a high concentration of particles derived from these sources in the air. The exposure to other animals such as horses, cows or pigs was lower. The differences between the epidemiological data reported by the Ministry of Health and those found in this study may be explained by the fact that the Ministry reported the census from the general population while our data corresponded to a population with suspected asthma, rhinitis or conjunctivitis. In patients with these diseases, physicians commonly recommend avoiding pets even without proof of clinical relevance.
We observed a high sensitization to birds, dogs and cats among patients with asthma, rhinitis and conjunctivitis, which correlates with the high frequency of these pets in the geographical region, and with patients´ exposure. We observed no direct relationship between frequent exposure to cats or dogs and sensitization. This may be explained by the high frequency of indirect exposure at school, work or in neighborhoods, which is difficult to quantify, but is probably high in the country considering the epidemiological data reported. Since dogs and cats share some allergenic proteins, principally from the lipocalin family, (13) this situation favors sensitization to both pets even in patients that may have little or no exposure at all to one of these two animals. According to clinical histories, 78% of patients sensitized to an animal were sensitized to the one they suspected was the trigger. Clinical histories are useful tools to identify suspects; however, they are not specific enough, especially if there has been perennial exposure to the allergenic source and the disease is chronic and multifactorial, as is the case of rhinitis, conjunctivitis and asthma.
It should be noted that the only way to find out with certainty the number of allergic patients to animals (or other sources) is using a provocation test, considered as the diagnostic gold standard, but this procedure was not performed routinely. One of the objectives of the study was to evaluate the effectiveness of pet avoidance on patients´ clinical response; however, only six of all the patients who had pets at home and were sensitized to them followed the recommendation of removing their pets from home and, therefore, it was not possible to carry out the analysis required to draw conclusions. Among patients with high indirect exposure, most of them said that they tried to reduce the contact with pets (94%), but during follow-up, 84% of them said they could not avoid exposure to animals due to the high presence of animals in most social areas (relatives´ homes, school, neighborhood).
There is scarce research about sensitization to birds; most of the studies were undertaken more than 20 years ago and reported a frequency of sensitization of 20 %, (14,15) which is high and seemed to have been caused by the extracts used in these studies, since they were contaminated with mite proteins. (16-18) Few recent studies have resorted to more purified extracts and there is controversy on whether sensitization to birds is relevant (5,19) or not (20) in allergic diseases. Findings showed that allergens present in bird droppings were more sensitizing than those in feathers, and that a relationship existed between having birds at home and sensitization. The frequency of sensitization to birds was over 10%, but sensitization to hens, doves, parakeets or canaries taken separately was less than 5%. This lower frequency of sensitization compared to that reported to cats or dogs may be explained by the small amount of people with birds as pets. There is little evidence of cross-reactivity between allergens from birds and from other pets like cats or dogs, therefore, direct exposure to birds could have a more relevant role (p=0.01). The smaller amount of patients sensitized to other sources such as hamsters, cows, and rabbits may be explained by the smaller amount of subjects tested for this and the reduced exposure to these animals in our city. We observed a low frequency of sensitization to horses, maybe due to the lack of exposure. Nevertheless, some people in the Aburrá Valley are highly exposed to horses, and, therefore, sensitization in this group could be higher than in the general population.
Environmental control measures refer to using one or more interventions aimed at avoiding, reducing or eliminating allergens and irritants in the environment. Most guidelines on allergic diseases recommend avoidance of sources of allergens as a logical and necessary step for symptom control. However, for perennial sources, the complete elimination of allergens is frequently impractical or even impossible. With pets, avoidance measures had their own challenges since most sensitized patients are not willing to remove their pets from home despite having a demonstrated sensitization. In fact, prior to performing the prick test in this study, two-thirds of patients with pets at home reported an unwillingness to remove them even if the tests were positive (data not shown). In addition, most patients reported having frequent exposure to animals at work, home or in their neighborhood, therefore, avoiding pets at home only partially reduces the exposure to animals.
Due to the high frequency of polysensitization in our patients, it is difficult to assess the clinical potential impact of avoidance measures to a specific source of allergens. Another important factor to consider is that sensitization to pets is not always clinically relevant and, therefore, avoidance measures sometimes are not necessary and may cause emotional problems. A provocation test would discriminate patients with clinically relevant sensitizations, but it is not routinely recommended due to the risk of severe reactions and technical difficulties. Based on results, such test is only suggested in sensitized patients with an unclear history in whom immunotherapy may be a treatment option. This test can help to determine whether removing pets from home could have some benefits or not, but since indirect exposure is common in many cities, (21) immunotherapy in patients with positive results in the allergic test should be considered in order to achieve a significant clinical impact.
Given our study design and the population selected, it was difficult to establish a relationship between sensitization and allergic symptoms. It would have been interesting to evaluate if some factors as exposure time or closeness to exposure sources could have influenced the severity of clinical response. Further studies in the general population would be required to evaluate the relationship between allergic diseases, sensitization and high exposure to pets.
In conclusion, it was not possible to evaluate the effectiveness of animal avoidance recommendations since most patients sensitized to animals at home were not willing to remove their pets. No clear relationship between household pets and the risk of sensitization was observed, which allows for the conclusion that it may occur due to high indirect exposure. Avoidance measures are difficult to implement because of the high emotional attachment to pets and indirect exposure, and, therefore, immunotherapy could be a management alternative.
In memory of Elizabeth López, MD, who contributed to data organization and collection for the article. We also want to thank Andrés Sánchez for revising the manuscript.
The authors declare no conflict of interests.
The study was funded by the Grupo de Alergología Clínica y Experimental, Universidad de Antioquia, Medellín, Colombia.
Corresponding author: Jorge Sánchez, Carrera 42 N° 7ª Sur- 92, bloque 3, apartamento 1710, Medellín, Colombia Teléfono: (300) 393 4000 jotamsc@yahoo.com
1. Dennis RJ, Caraballo L, García E, Rojas MX, Rondón MA, Pérez A, et al . Prevalence of asthma and other allergic conditions in Colombia 2009-2010: A cross-sectional study. BMC Pulm Med. 2012;12:17. http://dx.doi.org/10.1186/1471-2466-12-17
2. Macías-Weinmann A, Escamilla-Weinmann C, Pazos- Salazar NG, Valdés-Burnes DA, González-Díaz SN. Sensitivity to animals´ allergens in people working with animals. Rev Alerg Mex. 2010;57:185-9.
3. De Jong AB, Dikkeschei LD, Brand PL. Sensitization patterns to food and inhalant allergens in childhood: A comparison of non-sensitized, monosensitized, and polysensitized children. Pediatr Allergy Immunol. 2011;22: 166-71. http://dx.doi.org/10.1111/j.1399-3038.2010.00993.x
4. Burbach G, Heinzerling L, Edenharter G, Bachert C, Bindslev-Jensen C, Bonini S, et al . GA(2)LEN skin test study II: Clinical relevance of inhalant allergen sensitizations in Europe. Allergy. 2009;64:1507-15. http://dx.doi.org/10.1111/j.1398-9995.2009.02089.x
5. Sánchez J, Díez S, Cardona R. Sensibilización a aeroalérgenos en pacientes alérgicos de Medellín, Colombia. Rev Alerg Mex. 2012;59:139-47.
6. Brozek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, et al . Allergic rhinitis and its Impact on asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010;126:466-76. http://dx.doi.org/10.1016/j.jaci.2010.06.047
7. Santos MS, Alves MR, Freitas D, Sousa LB, Wainsztein R, Kandelman S, et al . Ocular allergy Latin American consensus. Arq Bras Oftalmol. 2011;74:452-6. http://dx.doi.org/10.1590/S0004-27492011000600016
8. Hanifin JM. Diagnostic criteria for atopic dermatitis: Consider the context. Arch Dermatol. 1999;135:1551.
9. Heinzerling LM, Burbach GJ, Edenharter G, Bachert C, Bindslev-Jensen C, Bonini S, et al . GA(2)LEN skin test study I: GA(2)LEN harmonization of skin prick testing: Novel sensitization patterns for inhalant allergens in Europe. Allergy. 2009;64:1498-506. http://dx.doi.org/10.1111/j.1398-9995.2009.02093.x
10. D e Knop KJ, Verweij MM, Grimmelikhuijsen M, Philipse E, Hagendorens MM, Bridts CH, et al . Age-related sensitization profiles for hazelnut ( Corylus avellana ) in a birch-endemic region. Pediatr Allergy Immunol. 2011; 22:e139-49. http://dx.doi.org/10.1111/j.1399-3038.2011.01112.x
11. Matricardi PM, Bockelbrink A, Beyer K, Keil T, Niggemann B, Grüber C, et al . Primary versus secondary immunoglobulin E sensitization to soy and wheat in the MultiCentre Allergy Study cohort. Clin Exp Allergy. 2008;38:493-500. http://dx.doi.org/10.1111/j.1365-2222.2007.02912.x
12. Liccardi G, Salzillo A, Piccolo A, D´Amato G. Skin prick test to horse should be included in the standard panel for the diagnosis of respiratory allergy. J Investig Allergol Clin Immunol. 2010;20:93-4.
13. Virtanen T, Kinnunen T, Rytkönen-Nissinen M. Mammalian lipocalin allergens--insights into their enigmatic allergenicity. Clin Exp Allergy. 2012;42:494-504. http://dx.doi.org/10.1111/j.1365-2222.2011.03903.x
14. Chapman JA, Williams S. Aeroallergens of the southeast Missouri area: A report of skin test frequencies and air sampling data. Ann Allergy. 1984;52:411-8.
15. von der Hardt H, Meiser W. Allergen testing in children with asthma bronchiale (author´s transl). Monatsschr Kinderheilkd. 1975;123:577-87.
16. Linna O, Niinimäki A, Mäkinen-Kiljunen S. Immunologic cross-reactivity between hen´s feather and house-dust-mite allergen extracts. Allergy. 1994;49:795-6.
17. Kemp TJ, Siebers RW, Fishwick D, O´Grady GB, Fitzharris P, Crane J. House dust mite allergen in pillows. BMJ. 1996;313:916. http://dx.doi.org/10.1136/bmj.313.7062.916
18. Colloff MJ, Merrett TG, Merrett J, McSharry C, Boyd G. Feather mites are potentially an important source of allergens for pigeon and budgerigar keepers. Clin Exp Allergy. 1997;27:60-7.
19. Sánchez J, Díez S, Cardona R. Frequency of sensitization to animals in a tropical area. Rev Alerg Mex. 2014;61:81-9.
20. Kilpiö K, Mäkinen-Kiljunen S, Haahtela T, Hannuksela M. Allergy to feathers. Allergy. 1998;53:159-64.
21. Simpson A. Ef fect of household pet ownership on infant immune response and subsequent sensitization. J Asthma Allergy. 2010;3:131-7. http://dx.doi.org/10.2147/JAA.S6958