Toxoplasmosis cerebral congénita e infección por el virus del Zika y del chikunguña: reporte de un caso
Resumen
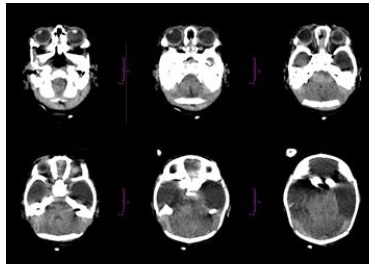
En este artículo se describe el caso clínico de una mujer colombiana del sur del país con diagnóstico de infección intrauterina por Toxoplasma gondii y por los virus del chikungunya y del Zika. La mujer acudió al control prenatal en el segundo trimestre de su embarazo e informó que durante el primer trimestre había presentado síntomas indicativos de infección por el virus del Zika. Mediante reacción en cadena de la polimerasa (PCR) en líquido amniótico, se demostró infección por Toxoplasma gondii así como por los virus del chikungunya y del Zika. En las imágenes diagnósticas se observaron malformaciones del sistema nervioso central en el feto. A las 29 semanas de gestación se dio por terminado el embarazo mediante procedimiento médico.
Descargas
Referencias bibliográficas
Carletti A, Gandolfi G, Perolo A, Simonazzi G, Ghi T, Rizzo N, et al. Prenatal diagnosis of cerebral lesions acquired in utero and with a late appearance. Prenat Diagn. 2009;29:389-95. https://doi.org/10.1002/pd.2244
Álvarez C, De la Torre A, Vargas M, Herrera C, Uribe-Huertas L, Lora F, et al. Striking divergence in toxoplasma-ROP16 nucleotide sequences from human and meat samples. J Infect Dis. 2015;211:2006-13. https://doi.org/10.1093/infdis/jiu833
De la Torre A, Sauer A, Bourcier T, Speeg-Schatz C, Ballonzoli L, Ajzenberg D, et al. Severe southamerican ocular toxoplasmosis is associated with decreased IFNgamma/IL-17A and increased IL-6/IL-13 intraocular levels.PLoS Negl Trop Dis. 2013;7:e2541. https://doi.org/10.1371/journal.pntd.0002541
Sánchez V, De la Torre A, Gómez-Marín JE. Characterization of ROP18 alleles in human toxoplasmosis. Parasitol Int. 2014;63:463-9. https://doi.org/10.1016/j.parint.2013.10.012
Peyron F, Lobry JR, Musset K, Ferrandiz J, Gómez-Marín JE, Petersen E, et al. Serotyping of Toxoplasma gondii in chronically infected pregnant women: Predominance of type II in Europe and types I and III in Colombia (South America). Microbes Infect. 2006;8:2333-40. https://doi.org/10.1016/j.micinf.2006.03.023
Rosso F, Agudelo A, Isaza Á, Montoya J. Toxoplasmosis congénita: aspectos clínicos y epidemiológicos de la infección durante el embarazo. Colomb Med (Cali). 2007;38:316-37.
Robert-Gangneux F, Dardé M. Epidemiology of and diagnostic strategies for toxoplasmosis. Clin Microbiol Rev. 2012;2:264-96. https://doi.org:10.1128/CMR.05013-11
Dunn D, Wallon M, Peyron F, Petersen E, Peckham C, Gilbert R. Mother-to-child transmission of toxoplasmosis: Risk estimates for clinical counselling. Lancet. 1999;353:1829-33. https://doi.org/10.1016/S0140-6736(98)08220-8
Desmonts G, Couvreur J. Congenital toxoplasmosis. A prospective study of 378 pregnancies. N Engl J Med. 1974;290:1110-6. https://doi.org/10.1056/NEJM197405162902003
Remington JS, McLeod R, Thulliez P, Desmonts G. Toxoplasmosis. En: Remington JS, Klein J, editores. Infectious diseases of the fetus and newborn infant, 5th edition. Philadelphia, PA: WB Saunders; 2001, p. 205-346.
Torgerson P, Mastroiacovo P. The global burden of congenital toxoplasmosis: A systematic review. Bull World Health Organ. 2013;91:501-8. https://doi.org/10.2471/BLT.12.111732
Burt FJ, Rolph MS, Rulli NE, Mahalingam S, Heise MT. Chikungunya: A re-emerging virus. Lancet. 2012;379:662-71. https://doi.org/10.1016/S0140-6736(11)60281-X
Ramful D, Carbonnier M, Pasquet M, Bouhmani B, Ghazouani J, Noormahomed T, et al. Mother-to-child transmission of Chikungunya virus infection. Pediatr Infect Dis J. 2007;26:811-5. https://doi.org/10.1097/INF.0b013e3180616d4f
Gérardin P, Barau G, Michault A, Bintner M, Randrianaivo H, Choker G, et al. Multidisciplinary prospective study of mother-to-child chikungunya virus infections on the island of La Reunion. PLoS Med. 2008;5:e60. https://doi.org/10.1371/journal.pmed.0050060
Senanayake MP, Senanayake SM, Vidanage KK, Gunasena S, Lamabadusuriya SP. Vertical transmission in chikungunya infection. Ceylon Med J. 2009;54:47-50
Shrivastava A, Wagar Beg M, Gujrati C, Gopalan N, Rao PV. Management of a vertically transmitted neonatal chikungunya thrombocytopenia. Indian J Pediatr. 2011;78:1008-9. https://doi.org/10.1007/s12098-011-0371-7
Fritel X, Rollot O, Gerardin P, Gauzere BA, Bideault J, Lagarde L, et al. Chikungunya virus infection during pregnancy, Réunion, France, 2006. Emerg Infect Dis. 2010;16:418-25. https://doi.org/10.3201/eid1603.091403
Besnard M, Eyrolle-Guignot D, Guillemette-Artur P, Lastère S, Bost-Bezeaud F, Marcelis L, et al. Congenital cerebral malformations and dysfunction in fetuses and newborns following the 2013 to 2014 Zika virus epidemic in French Polynesia. Euro Surveill. 2016;21. https://doi.org/10.2807/1560-7917.ES.2016.21.13.30181
Miranda-Filho DB, Martelli CM, Ximenes RA, Araújo TV, Rocha MA, Ramos RC, et al. Initial description of the presumed congenital Zika syndrome. Am J Public Health. 2016;106:598-600. https://doi.org/10.2105/AJPH.2016.303115
Barton M, Salvadori M. Zika virus and microcephaly. CMAJ. 2016;188:E118-9. https://doi.org/10.1503/cmaj.160179 21. Organización Panamericana de la Salud-Organización Mundial de la Salud. Zika - Actualización epidemiológica. 30 de junio de 2016. Fecha de consulta: 22 de septiembre de 2016. Disponible en: http://www.paho.org/hq/index.php?option=com_docman&task=doc_view&Itemid=
&gid=35265&lang=es
Corte Constitucional de Colombia. Sentencia C-355/06. Fecha de consulta: 28 de agosto de 2016. Disponible en: www.corteconstitucional.gov.co/relatoria/2006/C-355-06.htm.
Juliao O, Corredor A, Moreno G. Estudio Nacional de Salud: toxoplasmosis en Colombia. Bogotá: Instituto Nacional de Salud; 1988.
Gómez J. Toxoplasmosis: un problema de salud pública en Colombia. Rev Salud Pública. 2002;4(Supl.1):7-10.
Waggoner J, Gresh L, Vargas M, Ballesteros G, Téllez Y, Soda K, et al. Viremia and clinical presentation in Nicaraguan patients infected with Zika virus, chikungunya virus, and dengue virus. Clin Infect Dis. 2016;63:1584-90. https://doi.org/10.1093/cid/ciw589
Zambrano H, Waggoner J, Almeida C, Rivera L, Benjamin J, Pinsky B. Zika virus and chikungunya virus coinfections: A series of three cases from a single center in Ecuador. Am J Trop Med Hyg. 2016;95:894-6. https://doi.org/10.4269/ajtmh.16-0323
Sardi S, Somasekar S, Naccache S, Bandeira A, Tauro L, Campos G, et al. Coinfections of Zika and Chikungunya viruses in Bahia, Brazil, identified by metagenomic nextgeneration
sequencing. J Clin Microbiol. 2016;54:2348-53. https://doi.org/10.1128/JCM.00877-16
Cherabuddi K, Iovine N, Shah K, White S, Paisie T, Salemi M, et al. Zika and Chikungunya virus co-infection in a traveller returning from Colombia, 2016: Virus isolation and genetic analysis. JMM Case Rep. 2016;19:3:e005072. https://doi.org/10.1099/jmmcr.0.005072
Elbez-Rubinstein A, Ajzenberg D, Dardé ML, Cohen R, Dumètre A, Yera H, et al. Congenital toxoplasmosis and reinfection during pregnancy: Case report, strain characterization, experimental model of reinfection, and review. J Infect Dis. 2009;199:280-5. https://doi.org/10.1086/595793
Valdés V, Legagneur H, Watrin V, Paris L, Hascoët JM. Toxoplasmose congénitale secondaire à une reinfection maternelle pendant la grossesse. Arch Pediatr. 2011;18:761-3. https://doi.org/10.1016/j.arcped.2011.04.011
Gavinet MF, Robert F, Firtion G, Delouvrier E, Hennequin C, Maurin JR, et al. Congenital toxoplasmosis due to maternal reinfection during pregnancy. J Clin Microbiol. 1997;35:1276-7.
Lago EG, Baldisserotto M, Hoefel Filho JR, Santiago D, Jungblut R. Agreement between ultrasonography and computed tomography in detecting intracranial calcifications in congenital toxoplasmosis. Clin Radiol. 2007;62:1004-11. https://doi.org/10.1016/j.crad.2007.05.001
Diebler C, Dusser A, Dulac O. Congenital toxoplasmosis. Clinical and neuroradiological evaluation of the cerebral lesions. Neuroradiology. 1985;27:125-30.
Sabin A, Eichenwald H, Feldman H, Jacobs L. Present status of clinical manifestations of toxoplasmosis in man. Indications and provisions for routine serologic diagnosis. J Am Med Assoc. 1952;150:1063-9.
Arpino C, Curatolo P, Rezza G. Chikungunya and the nervous system: What we do and do not know. Rev Med Virol. 2009;19:121-9. https://doi.org/10.1002/rmv.606
Brito C. Zika virus: A new chapter in the history of medicine. Acta Med Port. 2015;28:679-80.
Kleber de Oliveira W, Cortez-Escalante J, De Oliveira WT, do Carmo GM, Henriques CM, Coelho GE, et al. Increase in reported prevalence of microcephaly in infants born to women living in areas with confirmed Zika virus transmission during the first trimester of pregnancy - Brazil, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:242-7. https://doi.org/10.15585/mmwr.mm6509e2
Malinger G, Werner H, Rodríguez-Leonel JC, Rebolledo M, Duque M, Mizyrycki S. Prenatal brain imaging in congenital toxoplasmosis. Prenat Diagn. 2011;31:881-6. https://doi.org/10.1002/pd.2795
D’Ercole C, Girard N, Boubli L, Potier A, Chagnon C, Raybaud C, et al. Prenatal diagnosis of fetal cerebral abnormalities by ultrasonography and magnetic resonance imaging. Eur J Obstet Gynecol Reprod Biol. 1993;50:177-84. https://doi.org/10.1016/0028-2243(93)90198-L
Barkovich AJ, Girard N. Fetal brain infections. Childs Nerv Syst. 2003;19:501-7. https://doi.org/10.1007/s00381-003-0763-8
Capobiango JD, Breganó RM, Navarro IT, Rezende Neto CP, Casella AM, Mori FM, et al. Congenital toxoplasmosis in a reference center of Paraná, Southern Brazil. Braz J Infect Dis. 2014;18:364-71. https://doi.org/10.1016/j.bjid.2013.11.009
Kıroğlu Y, Callı C, Karabulut N, Oncel C. Intracranial calcifications on CT. Diagn Interv Radiol. 2010;16:263-9. https://doi.org/10.4261/1305-3825.DIR.2626-09.1
Robin S, Ramful D, Le Seach F, Jaffar-Bandjee MC, Rigou G, Alessandri JL. Neurologic manifestations of pediatric chikungunya infection. J Child Neurol. 2008;23:1028-35.
https://doi.org/10.1177/0883073808314151
De Fatima Vasco Aragao M, van der Linden V, Brainer-Lima AM, Coeli RR, Rocha MA, Sobral da Silva P, et al. Clinical features and neuroimaging (CT and MRI) findings in presumed Zika virus related congenital infection and microcephaly: Retrospective case series study. BMJ. 2016;6:353:i1901. https://doi.org/10.1136/bmj.i1901
Hazin AN, Poretti A, Turchi-Martelli CM, Huisman TA, Microcephaly Epidemic Research Group, Di Cavalcanti Souza Cruz D, et al. Computed tomographic findings in microcephaly associated with Zika virus. N Engl J Med. 2016;374:2193-5. https://doi.org/10.1056/NEJMc1603617
Oliveira Melo AS, Malinger G, Ximenes R, Szejnfeld PO, Alves Sampaio S, Bispo de Filippis AM. Zika virus intrauterine infection causes fetal brain abnormality and microcephaly: Tip of the iceberg? Ultrasound Obstet Gynecol. 2016;47:6-7. https://doi.org/10.1002/uog.15831
Cavalheiro S, López A, Serra S, Da Cunha A, da Costa MD, Moron A, et al. Microcephaly and Zika virus: Neonatal neuroradiological aspects. Childs Nerv Syst. 2016;32:1057-60. https://doi.org/10.1007/s00381-016-3074-6
Faye O, Freire CC, Iamarino A, Faye O, de Oliveira JV, Diallo M, et al. Molecular evolution of Zika virus during its emergence in the 20th century. PLoS Negl Trop Dis. 2014;8:e2636. https://doi.org/10.1371/journal.pntd.0002636
Mlakar J, Korva M, Tul N, Popović M, Poljšak-Prijatelj M, Mraz J, et al. Zika virus associated with microcephaly. N Engl J Med. 2016;374:951-8. https://doi.org/10.1056/NEJMoa1600651
Algunos artículos similares:
- Wilber Gómez-Vargas, Kelly Valencia-Jiménez, Guillermo Correa-Londoño, Faiber Jaramillo-Yepes, Nuevas tabletas larvicidas de Bacillus thuringiensis var. israelensis: evaluación del efecto larvicida sobre Aedes aegypti (Diptera: Culicidae) en Colombia , Biomédica: Vol. 38 Núm. Sup. 2 (2018): Suplemento 2, Medicina tropical
- Jorge Hernán Montoya, Olga Lucía Morales, Reporte de cuatro casos de pacientes con síndrome de Jarcho-Levin en el departamento de Antioquia, Colombia , Biomédica: Vol. 29 Núm. 1 (2009)
- Ana Carolina Guimaraes, Ruy Lino-Junior, Virlanea Lima, Camila Cavellani, Rosana Rosa Corrêa, Mauricio Llaguno, Marlene Reis, Vicente Teixeira, Análisis epidemiológico de pacientes coinfectados con enfermedad de Chagas y cisticercosis , Biomédica: Vol. 29 Núm. 1 (2009)
- Claudia Blanco, María X. Núñez, Endoftalmitis por Pseudomonas aeruginosa posterior a queratoplastia penetrante, reporte de caso con investigación epidemiológica , Biomédica: Vol. 30 Núm. 3 (2010)
- Ana Cristina Restrepo, Jaime Alberto López, Perfil clínico y microbiológico de las lesiones por minas antipersonal en el Hospital Pablo Tobón Uribe, Medellín, 2003-2005 , Biomédica: Vol. 30 Núm. 3 (2010)
- Harry Pachajoa, Arelis Barragán, Javier Torres, Carolina Isaza, Pentalogía de Cantrell: reporte de un caso de padres consanguíneos , Biomédica: Vol. 30 Núm. 4 (2010)
- Edgar Martínez-Salazar, Alberto Tobón-Castaño, Silvia Blair, Malaria en humanos por infección natural con Plasmodium knowlesi , Biomédica: Vol. 32 (2012): Suplemento 1, Malaria
- Mariolga Berrizbeitia, Juan Luis Concepcion, Valentina Carzola, Jessicca Rodríguez, Ana Cáceres, Wilfredo Quiñones, Seroprevalence of T. cruzi infection in Canis familiaris, state of Sucre, Venezuela , Biomédica: Vol. 33 Núm. 2 (2013)
- Robson Paixão Souza, Joelma Nascimento Souza, Joelma Figueiredo Menezes, Leda Maria Alcântara, Neci Matos Soares, Márcia Cristina Aquino Teixeira, Infección humana por Trichostrongylus spp. en residentes de zonas urbanas de la ciudad de Salvador, Bahia, Brasil , Biomédica: Vol. 33 Núm. 3 (2013)
- Sergio Velásquez, Juan D. Matute, Laura Y. Gámez, Luis E. Enríquez, Iván D. Gómez, Fabiola Toro, Martha L. Valencia, Gisela De La Rosa, Pablo J. Patiño, Fabián A. Jaimes, Caracterización de la expresión de nCD64 en neutrófilos y de los niveles de s-TREM-1 y HMGB-1 en pacientes con sospecha de infección admitidos en el departamento de emergencias , Biomédica: Vol. 33 Núm. 4 (2013)
| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |

























