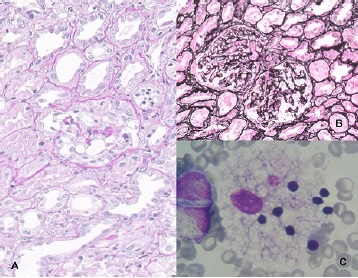
Glomerulonefritis colapsante con marcadores de desdiferenciación podocitaria en síndrome hemofagocítico secundario a linfoma hepatoesplénico de células T
Resumen
El síndrome hemofagocítico es una condición clínica e histológica grave, secundaria a diferentes procesos. La glomerulonefritis colapsante es una podocitopatía proliferativa, generalmente de pronóstico desfavorable para la función renal. Se presenta un caso en el que las dos condiciones aparecieron asociadas, lo cual es una forma infrecuente de presentación del linfoma hepatoesplénico de células T. Se discute, asimismo, el papel de los marcadores de desdiferenciación podocitaria en esta glomerulopatía, y se revisan la fisiopatología y el tratamiento.Descargas
Referencias bibliográficas
Fujiwara F, Hibi S, Imashuku S. Hypercytokinemia in hemophagocytic syndrome. Am J Pediatr Hematol Oncol. 1993;15:92-8.
Larroche C, Spivak JL. Pathogenesis of hemophagocytic syndrome. Autoimmune Rev. 2004;3:69-75. https://doi.org/10.1016/S1568-9972(03)00091-0
D´Agati VD, Fogo AB, Bruijin JA, Jenette JC. Pathologic classification of focal segmental glomerulosclerosis: A working proposal. Am J Kidney Dis. 2004;43:368-82. https://doi.org/10.1053/j.ajkd.2003.10.024
Verbsky JM, Grossman WJ. Hemophagocytic lymphohistiocytosis: Diagnosis, pathophysiology, treatment, and future perspectives. Ann Med. 2006;38:20-31. https://doi.
org/10.1080/07853890500465189
Kumukura S, Murakawa Y. Clinical characteristics and treatment outcomes of autoimmune-associated hemophagocytic syndrome in adults. Arthritis Rheumatol. 2014;66:2297-307. https://doi.org/10.1002/art.38672
Trottestam H, Horne A, Arico M, Egeler RM, Filipovich AH, Gadner H, et al. Chemoimmunotherapy for hemophagocytic lymphohistiocytosis: Long-term results of the HLH-94 treatment protocol. Blood. 2011;118:4577-84. https://doi.org/10.1182/blood-2011-06-356261
Aulagnon F, Lapidus N, Canet E, Galicier L, Boutboul D, Peraldi MN, et al. Acute kidney injury in adults with hemophagocytic lymphohistiocytosis. Am J Kidney Dis. 2015;65:851-9. https://doi.org/10.1053/j.ajkd.2014.10.012
Karras A. What nephrologists need to know about hemophagocytic syndrome. Nat Rev Nephrol. 2009;5:329-36. https://doi.org/10.1038/nrneph.2009.73
Málaga-Dieguez L, Ming W, Trachtman H. Direct reversible kidney injury in familial hemophagocytic lymphohistiocytosis type 3. J Am Soc Nephrol. 2015;26:1777-80. https://doi.org/10.1681/ASN.2014111090
Thaunat O, Delahoisse M, Fakhouri F, Martínez F, Stephan JL, Noël LH, et al. Nephrotic syndrome associated with hemophagocytic syndrome. Kidney Int. 2006;69:1892-
https://doi.org/10.1038/sj.ki.5000352
Esmaili H, Mostafidi E, Mehramuz B, Ardalan M, Mohajel-Shoja M. An update on renal involvement in hemophagocytic syndrome (macrophage activation syndrome). J Nephropathol. 2016;5:8-14. https://doi.org/10.15171/jnp.2016.02
Santoriello D, Hogan H, DÁgati VD. Hemophagocytic syndrome with histiocytic glomerulopathy and intraglomerular hemophagocytosis. Am J Kidney Dis. 2016;67:978-83.
https://doi.org/10.1053/j.ajkd.2015.11.017
Ponticelli C, Alberighi OD. Haemophagocytic syndrome--a life-threatening complication of renal transplantation. Nephrol Dial Transplant. 2009;24:2623-7. https://doi.org/10.1093/ndt/gfp282
Raffray L, Couzi L, Viallard JF, Pellegrin JL, Augis V, Vernant JP, et al. Mycophenolate mofetil: A possible cause of hemophagocytic syndrome following renal transplantation? Am J Transplant. 2010;10:2378-9. https://doi.org/10.1111/j.1600-6143.2010.03254.x
Nichols B, Jog P, Lee JH, Blackler D, Wilmot M, Dágit V, et al. Innate immunity pathways regulate the nephropathy gene apolipoprotein L1. Kidney Int. 2015;87:332-42. https://doi.org/10.1038/ki.2014.270
Genovese G, Tonna SJ, Know AU, Appel GB, Katz A, Bernhardy AJ, et al. A risk allele for focal segmental glomerulosclerosis in African Americans is located within a region containing APOL1 and MYH9. Kidney Int. 2010;78:698-704. https://doi.org/10.1038/ki.2010.251
Redondo-Pachón MD, Ortega-Salas R, Moyano-Peregrin C, López-Andreu M, Espinosa-Hernández M, Romera-Segorbe A, et al. Marcadores de desdiferenciacion podocitaria en un paciente con glomerulonefritis colapsante.Nefrología. 2010;30:360-6. https://doi.org/10.3265/Nefrologia.pre2010.Mar.10325
Albaqumi M, Barisoni L. Current views on collapsing glomerulopathy. J Am Soc Nephrol. 2008;19:1276-81. https://doi.org/10.1681/ASN.2007080926
Koukouritaki SB, Vardaki EA, Papakonstanti EA, Lianos E, Stournaras C, Emmanouel DS. TNF-alpha induces actin cytoskeleton reorganization in glomerular epithelial cells involving tyrosine phosphorylation of paxillin and focal adhesion kinase. Mol Med. 1999;5:382-92.
Markowitz GS, Nasr SH, Stokes MB, D´Agati VD. Treatment with IFN-{alpha}, -{beta}, or -{gamma} is associated with collapsing focal segmental glomerulosclerosis. Clin J Am Soc Nephrol. 2010;5:607-15. https://doi.org/10.2215/CJN.07311009
Pavenstadt H, Kriz W, Kretzler M. Cell biology of the glomerular podocyte. Physiol Rev. 2003;83:253-307. https://doi.org/10.1152/physrev.00020.2002
Shankland SJ, Eitner F, Hudkins KL, Goodpaster T, D´Agati V, Alpers CE. Differential expression of cyclindependent kinase inhibitors in human glomerular disease: Role in podocyte proliferation and maturation. Kidney Int. 2000;58:674-83. https://doi.org/10.1046/j.1523-1755.2000.00213.x
Barisona L, Nelson PJ. Collapsing glomerulopathy: An inflammatory podocytopathy? Curr Opin Nephrol Hypertens. 2007;16:192-5. https://doi.org/10.1097/MNH.0b 013e
b726b
Schwimmer JA, Markowitz GS, Valeri A, Appel GB. Collapsing glomerulopathy. Semin Nephrol. 2003;23:209-18.
Grcevska L, Polenakovik M. Collapsing glomerulopathy: Clinical characteristic and follow-up. Am J Kidney Dis. 1999;33:652-57. https://doi.org/10.1053/snep.2003.50019
Kashgary A, Sontrop JM, Li L, Al-Jaishi AA, Habibullah ZN, Alsolaimani R. The role of plasma exchange in treating post-transplant focal segmental glomerulosclerosis: A systematic review and meta-analysis of 77 case-reports and case-series. BMC Nephrol. 2016;17:104. https://doi.org/10.1186/s12882-016-0322-7
Asci G, Toz H, Ozkahya M, Cagirgan S, Duman S, Sezis M, et al. High-dose immunoglobulin therapy in renal transplant recipients with hemophagocytic histiocytic syndrome. J Nephrol. 2006;19:322-6.
Ferreri AJM, Govi S, Pilari SA. Hepatosplenic gamma-delta T-cell lymphoma. Crit Rev Oncol Hematol. 2012;83:283-292. https://doi.org/10.1016/j.critrevonc.2011.10.001
Han AR, Lee HR, Park BB, Hwang IG, Park S, Lee SC, et al. Lymphoma-associated hemophagocytic syndrome: Clinical features and treatment outcome. Ann Hematol. 2007;86:493-8. https://doi.org/10.1007/s00277-007-0278-6
Egües-Dubuc C, Aldasoro-Cáceres V, Uriarte-Ecenarro M, Errazquin-Aguirre N, Hernando-Rubio I, Meneses-Villalba CF, et al. Síndrome de activación macrofágica secundario a enfermedades autoinmunes, hematológicas, infecciosas y oncológicas. Serie de 13 casos clínicos y una revisión bibliográfica. Reumatol Clin. 2015;11:139-43. https://doi.org/10.1016/j.reuma.2014.06.007
Algunos artículos similares:
- Jorge de Jesús Cantillo, Rocío del Pilar López, Rafael Enrique Andrade, Enfermedad de depósito glomerular: a propósito de un caso de glomerulonefritis fibrilar , Biomédica: Vol. 29 Núm. 4 (2009)
- Leonardo F. Jurado, Andrés Gómez-Aldana, Mónica Tapias, Daniela Cáceres, Alonso Vera, Rocío del Pilar López-Panqueva, Rafael E. Andrade, Trastornos linfoproliferativos en una cohorte de pacientes adultos con trasplante hepático atendidos en un hospital de referencia en Bogotá, Colombia , Biomédica: Vol. 40 Núm. 3 (2020)
- Diana L. Franco, Sameer Islam, Kevin Ruff, Hallazgo endoscópico de linfoma folicular primario , Biomédica: Vol. 35 Núm. 1 (2015)
- John Fredy Nieto, Sandra Milena Gómez, Diana Carolina Moncada, Lina María Serna, Alicia Inés Hidrón, Tratamiento exitoso de linfohistiocitosis hemofagocítica y coagulación intravascular diseminada secundarias a histoplasmosis en un paciente con HIV/sida , Biomédica: Vol. 36 (2016): Suplemento 1, Microbiología médica
- Nicolás Villamizar-Rivera, Natalia Olaya , Experiencia en el uso de protocolos Biomed-2 para el estudio de reordenamientos de TCR e inmunoglobulinas en proliferaciones linfoides en el Instituto Nacional de Cancerología, Colombia , Biomédica: Vol. 42 Núm. Sp. 1 (2022): Mayo, Enfermedades crónicas en el trópico
| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |

























